COVID-19 and You
Last updated 4/28/2020

In December 2019, China reported an outbreak of upper respiratory illness called Coronavirus Disease (COVID-19) caused by a new coronavirus known as SARS-CoV-2. Since the announcement, the airborne virus has spread around the world, sickening more than a million people and killing thousands across the globe. It has also caused business and school closings, travel bans, and job loss.
Revelations about the virus and changes to social conventions are constantly evolving. Here’s what you need to know about how the virus infects humans and how to prevent further spreading.
Know your viruses
Coronaviruses are not new or unique, and there are hundreds of them. Some have caused symptoms of severe upper respiratory infections, such as SARS and MERS-CoV.
Coronaviruses are identified by the spikelike proteins that cover the external surfaces of the virus like a crown (hence the name). They are RNA viruses, which means their genetic makeup is RNA, as opposed to DNA. Because RNA lacks DNA’s “proofreading” mechanism, coronaviruses tend to mutate easily. Many originate in animals before developing a mutation that allows them to jump to humans.
There are seven coronaviruses that infect humans, resulting in colds, pneumonia, and bronchiolitis. Like all viruses, they act by entering and attaching to human cells, co-opting the host cell into reproducing their own RNA. The host cell ends up replicating the virus, which spreads throughout the body.
Although exposure to viruses often results in immunity, this is not always the case for coronaviruses. Because SARS-CoV-2 is completely new, almost no one has had a chance to develop the antibodies from infected people.
Know your risks
As of April 28, 2020, there were .3 million known COVID-19 cases worldwide, and 211,000 deaths. The SARS-CoV-2 virus can incubate for two days to two weeks before a carrier shows symptoms, during which time the person is contagious. According to the U.S. CDC, the most common symptoms are
- Fever
- Cough
- Shortness of breath
- Chills
- Repeated shaking with chills
- Muscle pain
- Headache
- Sore throat
- Loss of taste or smell
For most people, COVID-19 will feel like a bad cold or flu. But elderly (65+) and those with a compromised immune system, lung or heart conditions, or diabetes are at a higher risk for needing hospitalization. Over 80% of the deaths so far have been among the elderly, and they account for 45% of the hospitalizations and 53% of the intensive care admissions. One of the reasons Italy has suffered so much (12% death rate at the time of this article) is because it has one of the world's oldest population (oldest in Europe and second oldest in the world, behind Japan).
No one is sure why younger patients are less affected by the virus, but it likely has to do with the still-developing immune system in younger people. One hypothesis is that exposure to coronaviruses triggers the immune system to release cytokines, which cause much of the dangerous inflammation in the lungs; since the immune response is stronger each time you are exposed to a coronavirus, people who have not yet had much exposure have a reduced response.
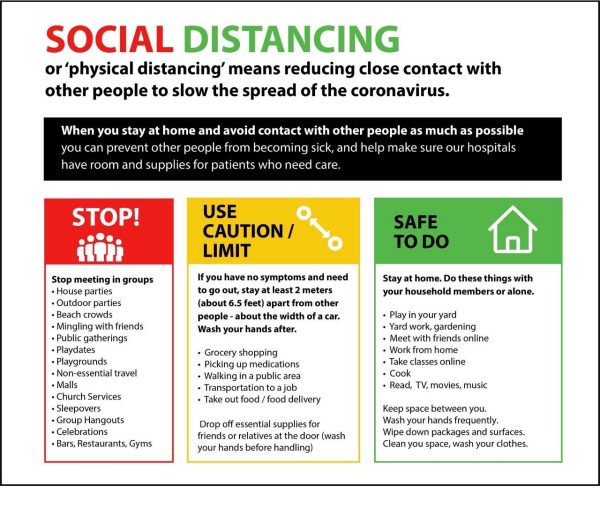
COVID-19 spreads via droplets expelled from the lungs when someone coughs or sneezes; keeping your distance from others (minimum of 6 ft or 2 m) prevents this type of transmission, though the virus is detectable in air for about 3 hours. It can also linger on hard surfaces for hours or days, so you can pick up the virus by touching a contaminated surface and then touching your eyes or mouth. Wash your hands frequently, use hand sanitizer (with at least 60% alcohol), and avoid touching your face.
Hunker down
Survial rate varies from country, and in places where the survival rate is high, the persistent calls for isolation and physical distance may seem like overkill. However, these measures are in place to combat two additional problems:
(1) Community spread: The initial cases of COVID-19 were easy to track. A patient had visited an infected area or had face-to-face contact with someone who did. But now, in many areas, the source of the contagion cannot be traced, which is referred to as community spread. Once this happens, the spread of the virus is much harder to control.
(2) Treatment availability: Suppose you live in an area with about 500,000 people, 15% of whom are over 65. If local hospitals have a combined 2,500 beds, and just 4% of the older people get sick at once, you’ll still have 500 senior citizens dying at home rather than getting medical care. And this doesn’t take into account the younger people that may require hospitalization for non-COVID-19-related illnesses: burst appendices, car accidents, and the myriad other reasons people go to the hospital.
In all likelihood, everyone will end up exposed to the virus at some point—the trick is to keep it from happening all at the same time so that doctors and hospitals can handle a manageable caseload. This is called flattening the curve, and it is the primary goal of all the lockdowns, school closures, and quarantines.
So, the lockdowns, online classes, and physical (social) distancing are more about protecting the community than protecting you (but staying safe is good, too).
It is entirely possible to be infected with the SARS-CoV-2 virus and not feel any symptoms, especially if you are young and healthy. So staying home and avoiding crowds is the best way you can help your community keep the spread of the disease manageable. And encourage others to do the same!
Diagnosis, treatments, and vaccines
The most common symptoms of COVID-19 are fever, dry cough, and shortness of breath, but a lot of illnesses share those symptoms. To determine whether your symptoms are caused by SARS-CoV-2, your doctor will start with a swab of your nose or throat. Many current test kits extract the RNA of any viruses on the swab, convert the RNA to DNA, and use fluorescent markers to bind to parts of the DNA unique to SARS-CoV-2. The DNA is then replicated until it can be detected by fluorescence spectroscopy.
Because RNA requires very specific conditions to replicate, analysis of the sample requires a specialty suite of chemicals that are suddenly in very high demand. Companies are ramping up production, but it will take time to provide tests for everyone who needs one.
At the moment, however, there is no vaccine for COVID-19, and the only treatment is rest and care. Moreover, any treatment identified would need to undergo months of trials for efficacy and safety, followed by more months to scale up production to the quantities needed to serve the population.
One shortcut to treatment is exploring off-label uses of old drugs. Because these medicines were already tested on humans, their side effects are well-known and documented; additionally, some are old enough that their patent protection has expired, allowing them to be produced at generic prices. Trials are under way to see if any could be effective against SARS-CoV-2.
Know what works to kill the virus
Standard disinfectants and soap are a great place to start. Bleach, hydrogen peroxide, and iso-propyl alcohol (rubbing alcohol) destroy the membranes that envelop bacteria and viruses. SARS-CoV-2 is no different. Although EPA regulations limit what manufacturers can state on their labels, properly used disinfectants will keep your surfaces (and hands) safe.
Commercial hand sanitizers can’t replace handwashing, but they are a good supplement to it. Granted, they are hard to come by right now. To that end, some distilleries are actually changing their operations to make the alcohols needed. Other manufacturers are also switching their equipment to produce needed supplies.
You also need to know what does and doesn’t work. Facemasks help to prevent you from sharing the virus. Gloves are useful but no substitute for frequent handwashing. There are no substances of any kind that you can ingest to protect yourself, even though that didn’t stop a man in Arizona man from overdosing on fish tank cleaner. Nor is there anything you should take, despite rumors surrounding known medicines.
It's best that you get medical information and guidance on how to protect yourself from your national public health organization.
Disease prevention and control centers around the world:
- Africa Centres for Disease Control
- European Centre for Disease Prevention and Control
- United States Centers for Disease Control
- Chinese Center for Disease Control and Prevention
Doing something… anything
Okay, so staying home doesn’t feel like you’re doing much to help. But it will feel better if you do something. Keep in touch with your friends. Use Zoom, FaceTime, Duo, or other video conferencing tools to have virtual parties (try houseparty), study sessions, or scavenger hunts. Make a TikTok video. Whatever it takes to connect with other people without actually being near them.
Want to do more? If you’re healthy, check with local organizations to see what they need. Foster a pet with your local animal shelter, raise money for a charity, sew masks for hospitals, or even donate blood. Check with your local church, food bank, or other community organization to find out how you can help support the elderly, low-income families, and those with chronic diseases in your neighborhood.
Make sure you are going through an organization though. They will help you with whatever arrangements are necessary to protect both you and the people they serve.
COVID-19 is scary, and times are going to be weird for a while. In the meantime, keep your sense of humor, keep your cool, and wash your hands.
Masks
Some countries began recommending the use of face coverings as a preventative measure. While there is little evidence that cloth face coverings prevent you from inhaling viruses, they have been shown to help prevent you from spreading viruses. Because you can spread SARS-CoV-2 without ever showing disease symptoms and the virus has been shown to travel farther than expected, face coverings can help slow the spread.
Washing your hands frequently and maintaining physical distance are still the most effective ways to keep the disease in check. Masks are supplement to this practice.
Here are a few tips for masks correctly.
- Make or purchase several reusable masks. Properly fitted N95 respirators and surgical masks provide better protection than general cloth masks, but they are desperately needed by medical staff and other front-line workers. Your best bet is to make or purchase several reusable masks that effectively block droplets, and use a fresh mask each time you need to go someplace. Wash the mask in your washing machine after each use.
- Completely cover your mouth and nose. You are trying to capture the virus-containing water droplets in your exhaled breath. The only way to do that is to keep your nose and mouth and keep covered.
- Do not touch your face while wearing or removing the mask. SARS-CoV-2 (as well as other viruses and bacteria) enters the body through your eyes, nose, and mouth. Keeping your hands away from these parts of your face helps reduce your chance of picking up or spreading the virus.
- Wash your hands and face after wearing the mask. Again, soap is a proven COVID-19 deterrent; use lots of it.