Checking Glycan Levels Could Catch Sepsis Before Symptoms Appear
Sepsis—an extreme inflammatory response in the bloodstream caused by a serious infection—could be responsible for as many as 11 million deaths worldwide per year, according to a 2020 report from the World Health Organization. Its incidence is also on the rise, driven by bacterial resistance to antibiotics. However, no biomarkers for the condition are known, which makes diagnosis difficult. A new study in mice suggests that changes in the blood levels of large sugar molecules known as glycans might play a role, which may open the door to new tests that could allow doctors to detect and treat sepsis at an early stage (ACS Infect. Dis. 2022, DOI: 10.1021/acsinfecdis.2c00082).
“There’s no molecular diagnosis for sepsis at the moment; it’s just a descriptive diagnosis,” says study coauthor Jamey D. Marth, director of the immunity and pathogenesis program at the research institute Sanford Burnham Prebys. That’s a problem because it means sepsis usually isn’t treated until its late stages when symptoms manifest.
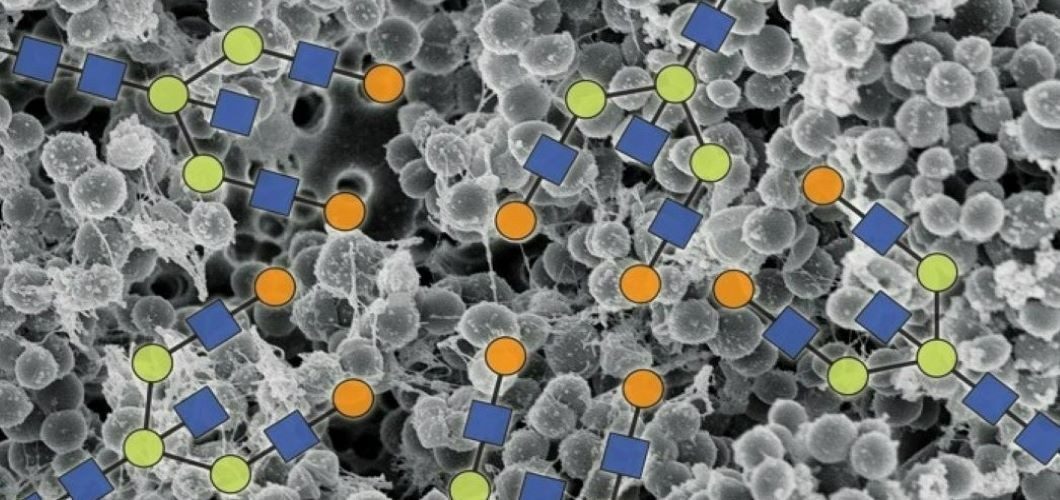
To identify potential molecular biomarkers, Marth and colleagues decided to focus on the glycome—the collection of an organism’s glycans that are either free floating or attached to proteins and lipids—because the glycome is already known to play a role in immunity and inflammation.
Glycans are already used as biomarkers for certain cancers, but the technology to study and measure them is relatively new and yet to be perfected. “We’re still not using glycans to their full potential,” says Ben Schumann, a chemical glycan biologist at Imperial College London and the Francis Crick Institute who was not involved in the study. There are vast amounts of still-unknown biology that affect and depend on the glycome, says Schumann, and a better understanding of the roles that glycans play could lead to new medical discoveries.
Marth’s team and Lara Mahal’s group at New York University induced sepsis in mice by infecting them with one of four strains of pathogenic bacteria: Streptococcus pneumonia, methicillin-resistant Staphylococcus aureus (MRSA), Escherichia coli, and Salmonella enterica. For each bacterial strain, the researchers collected blood from the mice and identified glycans in the samples.
The researchers observed significant changes in the glycomes that were consistent across all strains of bacteria. Levels of O-glycans—so called because they often link onto proteins’ oxygen-containing amino acids—in mice infected with MRSA were five times as high as those of uninfected mice. The other strains of bacteria led to O-glycan levels two to four times as high as an uninfected control. Meanwhile, concentrations of a glycan chains containing a branched structure known as a bisecting N-acetylglucosamine decreased by about 50% across all strains of bacteria.
Marco Jost, a microbiologist at Harvard Medical School thinks the approach is “solid, except that their infection doses seem very high.” Changes in the glycome might not happen at lower thresholds of bacterial infection, reducing the chances that measuring glycan levels could one day be used to diagnose sepsis in the crucial early stages of infection, Schumann says.
“It’s a good starting point to unravel what’s happening with sepsis,” Schumann says. Although the tools for probing the glycome are new, “I think we’re getting there.”
This article first appeared in Chemical & Engineering News on May 31, 2022.




